Patient education is key to driving better health outcomes and keeping people engaged.
But is your material up to mark? Or is it dry, boring, and lacking visuals? If so, attention-grabbing infographics are one of the best ways to improve your patient education efforts.
In this article, I’ll cover everything you need to know about using visuals to enhance patient teaching.
If you’re educating patients, making infographics is the way to go to make an impact in your patients’ lives.
Click to jump ahead:
- What is patient education?
- 5 types of patients
- 10 barriers to patient education
- 8 patient education examples
- What is a nurse’s role in patient education?
- Frequently asked questions
- Final words
What is patient education?
Patient education is the process of influencing patient behavior and producing the changes in knowledge, attitudes, and skills necessary to maintain or improve health.

About 6 in 10 Americans live with a chronic disease according to the Centers for Disease Control and Prevention (CDC). And these chronic conditions cost $4.1 trillion annually.
Patient education can help decrease this burden and inform people on chronic disease management.
Effective patient education requires educational material that is engaging (hint: visual content!).
According to a study in Frontiers Behavioral Neuroscience, 65% of people are visual learners.
That means text-heavy documentation or complex checklists will not engage patients. Instead your efforts should incorporate catchy infographics.
What are the 5 main types of patients?
Understanding patient’s needs can help you create the best patient education materials.
Here’s an overview infographic of the 5 types of patients:
1. Passive-dependent
Patients who are trusting individuals are passive-dependent.
They depend on a authoritative figure like healthcare professionals such as doctors and nurses to make their health decisions.
Passive-dependent patients can benefit from infographics featuring simple language and key takeaways.
2. Open-minded exploring
Patients who are open-minded exploring tend to look at health care as a collaboration between patients and doctors.
These patients seek a personal connection with a healthcare professional. They are usually open to exploring options for their health conditions, including alternative medicine and treatment plans.
Also, emotional support is important for this type of patient.
3. Independent-skeptical
Patients who always question doctors are independent-skeptical.
They don’t accept every recommendation and tend to seek second or even third opinions and chase after rational statements that are consistent with their knowledge.
4. Intellectual-researcher
Patients who always perform their literature search belong to this category.
They desire scientific explanations for every piece of information. They check their doctors’ comments against scientific studies and often prefer doctors who work in prestigious healthcare institutions.
5. Expedient-flexible
Patients who are expedient-flexible tend to choose family physicians based on current availability.
They don’t care much about educational resources or prestige. They are usually cost-conscious, which makes them flexible in their choice of physicians.
10 barriers to patient education
Providing detailed information about health is great, but clinicians and patients face several possible barriers that hinder educational efforts.
So what are the top 10 barriers to patient education? Let’s take a look.
1. Fear
Your patient may need to overcome fear before being open to receiving patient education handouts.
Scientifically, fear increases the human heart rate and produces a surge of stress hormones, which can hinder learning.
2. Receptive to teaching
Some patients embrace learning, but others need nudging and encouragement from their clinicians.
3. Health status
Adjust your patient education plan based on medical condition.
Materials about the early stage of a disease may not be beneficial if the patient’s disease has progressed.
4. Lack of time
Due to strict scheduling, physicians often do not have enough time to explain medical terminology.
The results of a focus group study showed that there is a big difference between learning for two hours and only having two or three minutes.
According to Krzywkowski-Mohn, patients feel “rushed and unable to voice all questions and concerns” when they have a short time with their doctors.
5. Complex issues
Patient education can be challenging because sometimes healthcare providers need to tackle multiple issues at once.
For example, to tackle obesity, you may need to discuss nutrition, exercise, peer influence, and stress from your patient’s circumstances.
6. Rising healthcare costs
In trying to save costs, patients tend to spend less time in the hospital before procedures such as surgery.
Therefore, nurses and physicians have less time to teach patients about such procedures.
7. Invisible results
Patients may not be interested in making changes to their health when there are no visible “dramatic results.”
For example, effective patient education may result in a heart attack that doesn’t occur or lung cancer that doesn’t form.
8. Licensing for telehealth services
It can be challenging for healthcare providers to get the licensing for telehealth services.
9. Capacity to handle information
Individuals have different limits when it comes to handling sensitive information. Providing patients only the amount of information they can handle at a time is an important aspect.
10. Lack of knowledge and skill level of health providers
Clinicians, nurses, and health educators need to keep updating their training on patient education.
Now that you know these barriers, what would be the right way to address them?
Make patient education materials with Venngage!
Infographics featuring pictures, drawings, and charts can make learning faster and address barriers such as insufficient time.
The simpler and catchier your visuals are, the easier patients can follow.
Also, by showing empathy in patient education visuals, you can alleviate the feeling of fear or concern that patients struggle with when they come into the doctor’s office.
This infographic highlights how common strokes are, but it also emphasizes that they can be prevented:
8 patient education examples
You’ll need different types of infographics to connect with the 5 patient types I mentioned above.
However, you should always create patient education content with these 8 tips in mind.
1. Use plain, non-medical language
Most people are not experts in medical lingo, so summarize medical concepts in simple terms.
Using simple, everyday language with visuals helps convey the message better and helps patients grasp information quickly.
For example, the infographic below uses simple language like, “Avoid sugar,” and “Stop biting your nails,” to help patients avoid getting sick.
2. Teach skills for self-management
For patients living with chronic conditions, your aim should be to educate them on how to live a complete life.
Self-management increases confidence, personal control, and self-efficacy.
The infographic below is a good example of visual you can use to help patients learn prevent and/or manage high cholesterol. how to live with diabetes.
3. Show or draw pictures
Creative images brings language to life and gets people’s attention, especially those who are visual learners.
Patient education is more impactful with pictures or drawings that support the text.
The infographic below makes use of an image of human anatomy to help educate people on what happens to a body exposed to drug use.
Related: How to Identify Patient Learning Styles: Teaching Patients More Effectively with Infographics
4. Use storytelling
Sometimes, numbers can look too complex to patients.
But using infographics or visual content is a great way tell a story with data.
Storytelling draws on emotions, which is one of the biggest motivators to learn.
Also, visual storytelling can help you accommodate for cultural differences, and promote tolerance, empathy, and sensitivity in patient education.
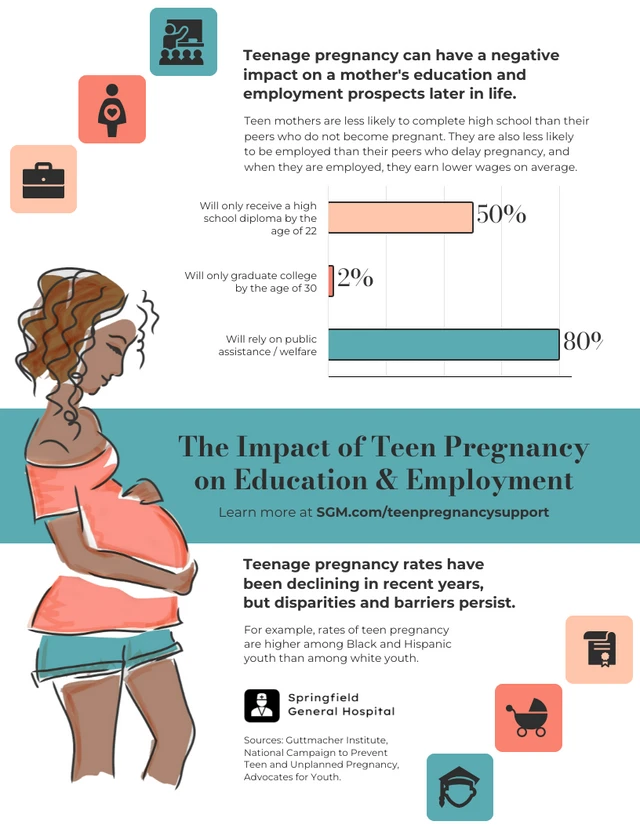
The infographic below shows how teenage pregnancy can negatively impact the mother in terms of education and employment. The use of a bar chart really helps drive the point home.
5. Use robust patient education materials
Everyone loves options!
One effective strategy in patient education is to provide multiple materials so that your patient can pick and choose based on their learning styles.
Patient teaching materials can include:
- Written materials
- Graphics (including infographics)
- Posters or charts
- Audiotapes/Podcasts
- YouTube videos
- Videotapes or DVDs
- PowerPoint presentations
- Demonstration using models or props
- Education portals
- Traditional lectures or group classes
- Verbal teaching
- Discussions
In addition to infographics, you can also other mediums for patient education like this poster:
6. Integrate modern methods of patient education
Patient education has evolved over the years.
Modern methods of patient education include:
- Technology resources: Patients can use their smartphones to find medical information on the web.
- Social media: Tech-savvy patients can consume health information from Social Media.
- Mobile health apps: These can work in conjunction with specialists to integrate support for the management of chronic diseases.
- Telehealth services: Clinicians can now educate patients via telehealth portals that include videos and messaging.
- Artificial intelligence (AI) solutions: Using AI, physicians can analyze patient data to personalize patient education.
Use visuals that point to other technology resources to help patients increase their knowledge by using smartphones or apps.
The infographic template below can teach your patients how to download a virtual healthcare app, which can help accelerate patient education.
7. Use the teach-back method
Patients often forget information after they are discharged.
And even when they recall some details, almost half of the recalled information is inaccurate.
So after you’ve used plain language to explain concepts to your patients, you should ask them to explain the details back to you in their own words. This technique is called the teach-back method.
Studies show that the teach-back method is an effective patient education strategy which leads to improved patient satisfaction with medication education, discharge information, and health management.
For example, after giving hand-washing instructions, you can ask patients to explain how they should wash their hands (and maybe even ask them what songs they’d like to use).
You can also send them the infographic below as a nice reminder:
8. Spend more time with patients
As challenging as health scheduling may be, healthcare providers need to increase the time spent with patients.
One study implemented a one-hour personalized session with a discharge nurse. The extra time spent with the patient results in the following benefits:
- Improved clinical outcomes: reduced re-hospitalization or death by 35%.
- Increased heart failure self-care practices: regular weight measurements, strict sodium restriction, and cessation of cigarette smoking.
- Reduced medical costs: reduction in re-hospitalization rates led to decreased medical costs (by $2,823) over the 180-day follow-up period.
What is a nurse’s role in patient education?
Nurses make up the bulk of healthcare professionsals.
Approximately 4.1 million nurses are registered RNs in the US. Therefore, nurses are critical to patient education.
Surprisingly, nurses have the highest rate of no prior health literacy knowledge of all medical professionals.
Healthcare institutions need to provide nurses with the necessary tools to assess patient health literacy.
To improve their role in patient education, nurses need to learn the following health literacy concepts:
Cultural competence
Cultural competence respects and considers a person’s cultural background, cultural beliefs, and values, and incorporates this knowledge into their health care.
Minorities often have language barriers.
Nurses can use resources for patients who do not speak the same languages as they do, for example, interpreter services.
Tools to assess patients’ health literacy levels
Some examples of assessment tools include the Test for Functional Health Literacy (TOFHLA) and the Rapid Estimate of Adult Literacy in Medicine (REALM).
Skills to handle patients with low health literacy
Nurses need to be aware that there are vulnerable populations with low health literacy.
The Agency for Healthcare Research and Quality (AHRQ) has developed a toolkit to help healthcare providers eliminate health literacy barriers.
Some recommendations in the AHRQ toolkit to reduce health literacy barriers include:
- Train one staff member to evaluate the quality of materials you give to patients.
- Check whether patient materials are easy to read and understand. You can use one of the assessments created by the AHRQ, the Centers for Diseases and Control (CDC), or the Suitability Assessment of Materials (SAM).
- Ask patients to evaluate your forms and other written materials. They may provide helpful insights for making these materials better.
- Watch out for numbers. Only include numbers that help make informed decisions.
Frequently Asked Questions
Why is patient education important?
Patient education is important because evidence points to the fact that patients who receive superior patient education enjoy better health outcomes.
What are the benefits of patient education?
The benefits of patient education include improved individual well-being and a better overall healthcare system. Here are the list of benefits in detail.
1. Patient education decreases anxiety
When patients have a high level of certainty, they are less anxious. Patient education materials can decrease anxiety by explaining warning signs and complications.
Of course, no one can ever be 100% certain or prepared. However, a high level of certainty makes patients more confident about what signs to watch for.
For example, the infographic below is helpful for quickly determining whether symptoms are COVID-19-related or from a common cold, flu, or allergies.
2. Patient education increases adherence and compliance
Patients differ in their abilities to understand and comply with health-related materials and instructions.
Helping patients understand their medical conditions increases engagement, which leads to adherence and compliance. A patient who understands the “why” is more inclined to follow the doctor’s orders.
3. Patient education increases symptom improvement
One study of asthma patients showed that the use of digital technology resources led to improvement in symptoms.
Patient education helps patients learn how to manage their chronic medical conditions.
For example, this patient education infographic tells patients how to manage high blood pressure.
4. Patient education increases knowledge
Patient education increases patients’ understanding of medical conditions.
Armed with the right knowledge, patients can improve their attitudes toward preventive health.
Knowledge also helps patients use the correct methods and procedures at home.
An example of patient education that increases knowledge is this infographic that educated patients on how to prevent catching and spreading the coronavirus during the pandemic.
5. Patient education increases satisfaction
Easy access to digital health resources (e-health) increases patient satisfaction.
Using patient education tools, clinicians can also help patients navigate the healthcare system and maintain their data.
Patients who are in control of their health and completely engaged in the decision-making process have a higher level of satisfaction.
6. Patient education reduces hospital readmission rates
About one in five patients discharged from hospitals have complications within 30 days resulting in visits to the emergency room (ER) or readmission.
One of the reasons for re-hospitalization is low health literacy.
Physicians and nurses should assess patients for health literacy and create patient education materials that are at various levels of literacy.
What is the first step in patient education?
The first step in patient education is to understand the health literacy level of your patient. Only after doing so can you match your patient education materials to their level of understanding and cultural beliefs.
What are the top 3 patient education topics?
On a global scale, most patient education resources cover these top 3 topics: physical activity, obesity, and tobacco use
What is the main purpose of patient education?
The main purpose of patient education is to help patients enjoy better health outcomes.
Patient education influences patients’ behaviors and motivates them to make changes in their knowledge, attitudes, and skills to help them maintain or improve their health.
What are the main patient education concepts?
The main patient education concept is to provide a framework for clinicians to teach patients.
Before you start teaching, get familiar with these patient education theoretical concepts:
1. Health literacy
According to WHO, health literacy “represents the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand, and use information in ways which promote and maintain good health.”
In 2011, about 80 million Americans had low health literacy. This is nearly half of all US adults.
However, not all physicians feel that health literacy is a major concern, and this needs to change.
In a survey, 77% of physicians felt that health literacy was only a moderate obstacle. But that’s not true. Health literacy can be a great obstacle.
Shockingly, patients may have a high overall literacy but still have a low health literacy.
People with low health literacy:
- Have poorer overall health
- Do not adhere to medications
- Use more health and emergency services
- Wait longer before seeking medical help
People with low health literacy “struggle with even the most basic tasks—for example, using a search function, navigating from a drop-down menu, and scanning a webpage for relevant information,” according to Health.gov.
Factors that affect health literacy include:
- Poverty
- Education
- Race/ethnicity
- Age
- Disability
2. The health belief model
Patients’ beliefs, whether religious, cultural, ethnic, or any other kind of belief, can shape how they understand and process health information.
The health belief model states that:
“A person’s belief in a personal threat of an illness or disease together with a person’s belief in the effectiveness of the recommended health behavior or action will predict the likelihood the person will adopt the behavior.”
Patients have different beliefs regarding childbirth, death, the role of women, and the role of family. To be more effective, you need to respectfully ask patients about their beliefs before devising a patient education strategy.
Using a patient education infographic like the Contraceptive Methods Comparison template below shows that you understand your patients may have different beliefs about the “best” method of contraception. This comparison infographic is a great way to get your patients talking and asking questions.
3. The rational model
This is also called the Knowledge, Attitudes, Practices (KAP) model. The rational model suggests that increasing a patient’s knowledge will motivate them to make a behavioral change.
However, knowledge alone is not sufficient. Make sure you supplement the rational model with other concepts.
4. The extended parallel processing model (EPPM)
The EPPM model is also called “threat management or fear management.” A person’s rational and emotional beliefs can combine to determine how they will respond to patient education.
If patients feel threatened, they will respond positively. If they don’t feel threatened, they may not adhere to medications or comply with the doctor’s orders.
Fear appealing campaigns work in health education. This is because people take preventive steps when they are afraid.
For example, the COVID-19 pandemic prompted clinicians and public health professionals to create several threat or fear management campaigns.
5. Communication theory
To provide effective patient education, you have to consider your targeted patient.
Communication theory is based on the premise that multilevel strategies are necessary depending on the person you are communicating with.
Patients have different levels of health literacy, so you should tailor your message to your specific patient.
The infographic below, Telemedicine in Your Community, is targeting patients who do not have any experience with telemedicine. Listing the steps to take, from checking wait times to starting your appointment, is helpful for new telemedicine patients.
For the full list of patient education concepts, check the World Health Organization (WHO) guide on health education.
In a nutshell: An effective patient education strategy is one that incorporates the use of visuals
Patient education goes beyond teaching patients about medical conditions.
Effective patient education influences and motivate people to make better-informed decisions about their health.
To provide the best patient education, healthcare providers must recognize that patients have various health care literacy levels and tailor their content to match it.
The most effective patient education strategies drive the following results: decreased anxiety, increased adherence and compliance, reduced hospital readmission rates, and better knowledge and satisfaction.
To start incorporating visuals to your patient education, jump right in and start making infographics with Venngage. You can start designing an engaging, memorable patient teaching material for free, no design experience required.